Is Sleep Apnea impacting your life?
You’ve heard of it, and likely know people who suffer from it. Untreated, it makes you 2-4x as likely to be involved in a car accident1, 3.7x as likely to suffer a stroke2, and 50% more likely to suffer psychological distress3. Roughly 25% of Canadian adults suffer from some form of Sleep Apnea, and yet only 20% of sufferers have been diagnosed5. So what’s happening with this common but under-recognized condition?
Understanding Sleep Apnea
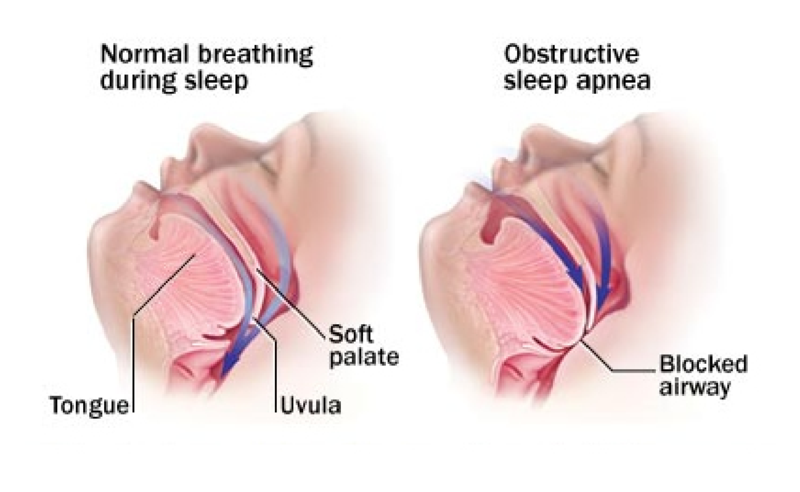
While awake, our throat muscles act to keep our airway open, making breathing easy and natural. During sleep, our muscles - including those in our throat - relax. In some people, this causes the airway to narrow or close, obstructing air flow. When this happens, our heart rate and blood pressure increase, blood oxygen levels drop, adrenaline surges, and our brain wakes us up to kick-start breathing again. In severe cases, this cycle can happen over 30 times per hour, putting significant strain on our cardiovascular system and preventing the deep, restorative sleep we need to function the next day.
Common Signs and Symptoms
- Excessive daytime sleepiness
- Irregular breathing during sleep (gasping, long pauses, shallow breathing)
- High blood pressure
- Poor memory / concentration
- Snoring
Diagnosis
The diagnosis of Sleep Apnea is done by an overnight Sleep Study. There are three common diagnostic test options:
Portable Home Sleep Testing. Your family doctor may provide you with a prescription for an at-home sleep study to diagnose sleep apnea. These tests usually involve oximetry, measurement of airflow and measurement of breathing patterns. These tests are excellent at determining if you have Obstructive Sleep Apnea and can be worn in the comfort of your own bed. Portable testing options are available here, and all include an interpretation and consultation with one of our Registered Respiratory Therapists following your results.
Nocturnal polysomnography. During this test, you're hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep. This can help your doctor rule out other conditions — such as periodic limb movements or narcolepsy — that can also cause excessive daytime sleepiness, but require different treatment. These tests must be done in an overnight sleep lab facility.
Oximetry. This screening method involves using a small machine that monitors and records your blood oxygen level while you're asleep. A simple sleeve fits painlessly over one of your fingers to collect the information overnight in a sleep lab. If you have sleep apnea, the results of this test will often show drops in your blood oxygen level during apneas and subsequent rises with awakenings.
If you think you may suffer from Sleep Apnea, talk to your family doctor about your options for diagnosis.
Therapy
The gold standard for treating Sleep Apnea is PAP Therapy (Positive Airway Pressure). With PAP, a small bedside device delivers positive airway pressure through a mask that you wear while you sleep. The air pressure acts as a splint to keep your airway open, preventing the collapse of the airway and allowing for full and normal breathing during sleep. Other treatment options include weight loss, oral appliances, or surgical procedures.
If you think you might suffer from Sleep Apnea, talk to your doctor today. Beyond the serious health consequences, there are huge productivity and lifestyle benefits from starting treatment. We hear from our patients all the time how much better life is on a good night’s sleep! So don’t wait! Call us today for a free consultation or to learn more about sleep and Sleep Apnea therapy.
Sources: 1. New England Journal of Medicine 2. American Academy of Sleep Medicine 3. Bernabe et. Al 2015 4. Young et. Al, University of Wisconsin School of Medicine and Public Health 5. Peppard et al. J Am Med Assoc 2013



